Osteoarthritis is the progressive non-inflammatory destruction of articular cartilage.
As a result of degenerative-dystrophic changes, the joint gradually loses its functions, flexion-extension movements in it become difficult and then completely impossible.
Joints are movable joints of bones. The human body contains more than 200 joints that provide all types of movements of the bony skeleton. Free sliding within them is carried out thanks to the smooth surfaces of the hyaline cartilage and synovial lubrication.
With osteoarthritis, the hyaline cartilage becomes thinner and gradually collapses, becomes rough, and synovial lubrication becomes insufficient for free flow. As a result, friction occurs which prevents the movement of the joint and leads to its progressive destruction.
Osteoarthritis is one of the most common degenerative-dystrophic diseases of the musculoskeletal system. They affect more than 30% of people between the ages of 45 and 65 and more than 65% of people over the age of 65. The incidence has a marked age dependency.
Most often, the disease affects large joints: knee (gonarthrosis), hip (coxarthrosis) and shoulder. Among the small joints, those most often affected are the joints of the hand, foot and spine.
In an advanced stage of the disease, ankylosis (complete immobilization) of the joint occurs. In this case, only surgical treatment is possible: removal and replacement with an endoprosthesis.
In stages 1 - 3 of arthrosis, conservative treatment is possible, the purpose of which is to slow down and stop the destruction of the joint, gradual restoration of cartilage tissue, improvement of functions (mobility), increased range of motion, pain relief symptoms and inflammation.
In the clinic these objectives are achieved through the integrated use of foot reflexology, herbal and physiotherapeutic methods of oriental medicine.
Causes of osteoarthritis
The cause of the disease is the predominance of wear and tear of hyaline cartilage over the regeneration process. This means that joint cartilage is worn down and destroyed under stress faster than it can recover.
This happens due to the action of two factors: increased loads and/or slow recovery.
For the regeneration of hyaline cartilage, collagen is needed, which is produced in the body with the participation of the liver.
This organ not only participates in the synthesis of collagen, which is necessary for joints, but is also responsible for the level of body heat.
From a medical point of view, the cause of all cold diseases, including arthrosis, is a decrease in the level of body heat. This can happen, in particular, due to insufficient liver function.
All arthrosis belongs to degenerative and dystrophic diseases. Their development begins with dystrophy, that is, tissue starvation due to insufficient blood supply.
To constantly regenerate, articular cartilage needs collagen, a universal building material of connective tissue. This protein substance is synthesized in the body and enters the joints with the blood.
If for some reason the blood supply is cut off, the hyaline cartilage lacks collagen. The regeneration process in them slows down. In this case, the joints that bear the greatest load – knees, ankles, hips and shoulders – suffer the most. The articular cartilage gradually begins to wear out and collapse.
When cartilage is destroyed, its fragments tear and move freely in the joint cavity (so-called "rats"), causing pinching, blockages, further limitations of movement and increased pain.
Another cause of the disease may be collagen deficiency due to insufficient synthesis of this substance in the body. This may be due, for example, to functional failure of the liver, which actively participates in this synthesis.
Provocative factors for the development of the disease can be:
- overweight,
- unhealthy diet
- heavy physical work, intense sports,
- trauma, multiple microtraumas,
- exposure to cold
- age-related changes (dehydration) in the body,
- congenital anomalies (dysplasia, weakness of connective tissues, etc. ).
Classification
Arthrosis that develops against the background of metabolic disorders is called primary.
Secondary arthrosis occurs against the background of inflammatory processes (arthritis, including autoimmune), endocrine diseases or injuries.
Some of the most common forms of the disease have their own names: gonarthrosis (knee joint), coxarthrosis (hip joint), spondyloarthrosis (spine).
With the addition of inflammation, the disease is diagnosed as arthrosis-arthritis.
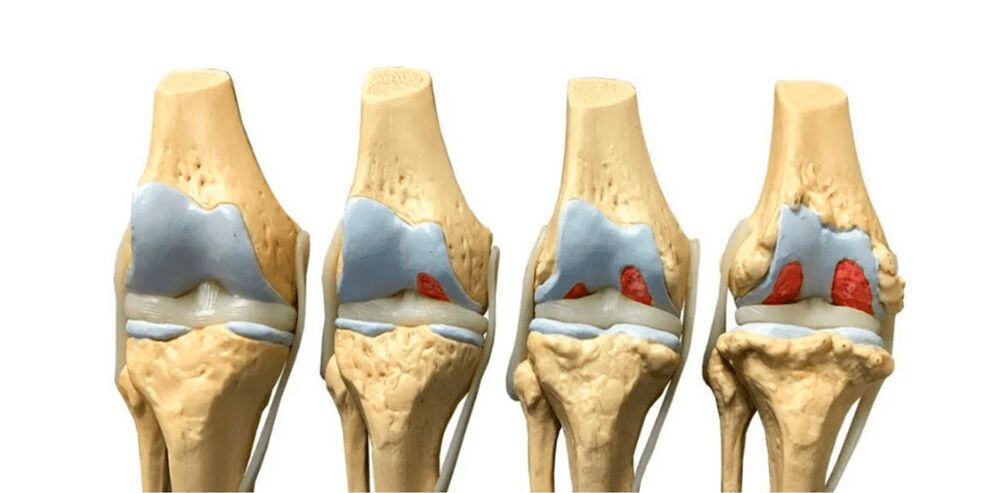
There are four stages in the development of the disease.
Arthritis of the 1st stage is manifested by periodic pain and slight narrowing of the joint space.
Stage 2 of the disease involves significant narrowing of the joint space, limited mobility, the formation of bony growths (osteophytes), and joint deformation.
Stage 3 arthrosis means almost complete disappearance of the joint space, limitation of the range of movement to a minimum, deformation of the joint, involvement of the periarticular tissues and bones (osteoarthrosis, periarthrosis).
At the 4th stage complete immobilization (ankylosis) occurs, the joint space disappears completely.
Symptoms of osteoarthritis
Like many other degenerative-dystrophic diseases of the musculoskeletal system, arthrosis develops gradually.
Symptoms may be absent for a long time, although changes in cartilage tissue, volume and synovial lubrication properties have already begun.
Symptoms of stage 1 arthrosis are increased fatigue in the joint, mild pain that occurs after physical activity or at the beginning of movements after long periods of immobility (the so-called "initial" pain), after of which the joint develops. The range of flexion-extension and rotation movements is not limited and there are no difficulties during the movements.
In phase 2, joint pain becomes more intense and lasts longer, manifesting itself even with lower loads. A squeaking or creaking sound is heard while moving. Flexion, extension and rotation movements become difficult, their volume is increasingly limited. Stiffness develops.
At the 3rd stage of osteoarthritis, joint pain becomes constant. Joint movements are performed with great difficulty, their volume is reduced to a minimum. The joint is severely deformed due to bone growth and increase in size. When the leg joints are affected, severe lameness develops.
In stages 2-3 of the disease, inflammation usually manifests itself with symptoms such as swelling, redness, increased pain and local fever.
Pain in arthrosis can intensify with changes in the weather, humidity, cold, at night, at the beginning of movement or during physical activity, as well as when the joint is clamped with a mouse.
Diagnostics
The diagnosis of arthrosis is made on the basis of a survey, external examination and hardware methods (X-ray, CT, MRI).
During the interview, the doctor studies the medical history, asks the patient about the symptoms, the circumstances of their appearance and exacerbation.
At the first appointment in the clinic, the doctor, as a rule, asks the patient not only about the symptoms of arthrosis, but also about the nature of nutrition and lifestyle, since in oriental medicine the human body is considered a single system. In this unified system there are internal relationships.
For example, the condition of the joints strictly depends on the metabolism, immune system, hormonal system, movement of body fluids and body mass index.
Modern medicine classifies arthrosis as a cold disease that develops against the background of energy depletion of the body, decreased heat levels and accumulation of cold. The key factors in this case are poor nutrition, sedentary lifestyle, exposure to cold and humidity.
During external examination, the doctor pays attention to the size, shape of the joints, range of motion, as well as signs of inflammation: swelling, redness, local increase in temperature.
After examining and interviewing the patient, the doctor sends him for further examination: x-ray, CT or MRI.
During an x-ray, the doctor sees a narrowing of the joint space, which indicates thinning of the cartilage. Based on the degree of narrowing, the stage of arthrosis is determined.
An X-ray image clearly shows osteophytes: growths along the edges of bones that form during osteoarthritis.
The x-ray visualizes the bone tissue well, but poorly shows the soft connective structures. Magnetic resonance imaging (MRI) provides much more information.
Using a tomogram, the doctor can examine in detail the condition of the hyaline cartilage, as well as the synovial bag, joint capsule and detect joint "mice", damage to the meniscus and ligaments.
To study the blood supply to the joint, angiography with a contrast agent (radiography, computed tomography or magnetic resonance imaging) is prescribed.
Treatment of osteoarthritis
At stage 4 of arthrosis, surgical treatment is used, the joint is removed and replaced with an endoprosthesis. In stages 1 - 3 of the disease, conservative treatment is carried out.
- Medicines.Drug therapy is used to relieve symptoms and slow the progression of the disease. In the presence of an inflammatory process, hormonal drugs (glucocorticoids) or non-steroidal drugs (NSAIDs based on ibuprofen, diclofenac, etc. ) are prescribed. Typically, these drugs are given by injection into a joint or intramuscularly. To slow down the process of destruction of articular cartilage, chondroprotectors are prescribed.
- Injections into the joint.To reduce friction and improve sliding, hyaluronic acid is injected into the joint cavity, whose molecules have the ability to retain moisture. Hyaluronic acid injections protect cartilage surfaces from dehydration and slow down their destruction.
In the presence of severe inflammation and swelling, injections of hormonal drugs into the joint cavity are used. - Operation.Surgical treatment of arthrosis consists of replacing the joint with an endoprosthesis. These interventions are indicated at the 4th stage of the disease with ankylosis (complete immobility).
- Physiotherapy.To relieve inflammation, physical therapy methods such as laser therapy, magnetic therapy and drug administration using current (electrophoresis) or ultrasound (phonophoresis) are used.
Mud applications, compresses and heating improve local blood circulation, promote healing and restoration of cartilage tissue and relieve pain. - Other treatments.To prevent arthrosis, as well as an auxiliary treatment method, physical therapy (exercise therapy) is prescribed. Regularly performing simple exercises improves blood flow to the joint, increases its mobility and range of motion.
Warm baths can be used to warm a sore joint and relieve symptoms. Balneological treatment for arthrosis includes remedies such as mud or radon baths.
It's important!
Chondroprotectors do not affect the causes of arthrosis. Essentially, these are not therapeutic agents, but prophylactics. They contain chondroitin and glucosamine, which work to increase the amount of lubrication (synovial fluid) and facilitate gliding. Reducing friction slows the destruction of cartilage, but does not restore it.
To not only slow down the development of the disease, but also reverse it, it is necessary to improve blood supply, activate the processes of metabolism and tissue regeneration. Chondroprotectors don't do this. Therefore they can be used as an aid, but not as a replacement for complete treatment.
Treatment of arthrosis in a specialized clinic
In the clinic, treatment of stage 1 - 3 arthrosis is carried out using phyto, physiological and reflexological methods of oriental medicine. Positive results are obtained in more than 90% of cases of treatment of this disease.
Complex treatment sessions include several procedures (moxibustion therapy, acupressure, acupuncture, etc. ), which mutually enhance the effect according to the principle of synergy.
Treatment in the clinic is aimed at eliminating the cause of arthrosis, this guarantees long-term and lasting results.
Joint diseases refer to disorders underlying the Bad Kan, one of the body's three control systems, whose balance means health and whose imbalance means disease. In addition to the joints, this base is responsible for the lymphatic system, body fluids, immunity, hormones and metabolism.
A Bad Kan imbalance usually causes not one, but several diseases at once. Therefore, arthrosis is almost always accompanied by concomitant disorders, diseases such as overweight (obesity), chronic respiratory diseases, allergies and/or immunodeficiency conditions, endocrine disorders, hormone-dependent gynecological diseases (in women), etc.
Modern treatment restores the balance of the Bad Kan base as a whole and thus eliminates the common cause of all these diseases. Therefore, along with arthrosis, other concomitant diseases also occur.
In the treatment of arthrosis, the doctor works not only on the affected joint area, but also on the body as a whole, in order to restore the balance of the Badk-an base. This is the secret of the high effectiveness of arthrosis treatment in our clinic.
Tszyu or moxo therapy.
This procedure consists of simultaneous or sequential heating of bioactive points with an absinthe cigar or smoking cones (made of wormwood or charcoal). Ju therapy is the main treatment for osteoarthritis in alternative medicine. It is used both locally, on the affected joint area, and on the body's meridians to restore balance to the Bad Kan base and the body as a whole.
This procedure has a global effect: improves blood circulation, stimulates blood flow, activates and accelerates the restoration and renewal of connective tissues, improves the properties and normalizes the volume of synovial lubrication, and has an anti-inflammatory and metabolic effect.
Acupuncture.
The introduction of medical needles into bioactive points has an anti-inflammatory, decongestant, analgesic effect and promotes the outflow of inflammatory fluid.
The impact on the bioactive points of the liver meridian helps to improve the functioning of this organ and activate collagen synthesis in the body.
The impact on the bioactive points of the kidneys helps to improve blood circulation in the lower part of the body in case of gonarthrosis, coxarthrosis and other arthrosis of the legs.
Acupressure.
Strong point pressure improves local circulation, increases blood flow, accelerates metabolic processes and tissue regeneration, eliminates muscle tension and spasms. Acupressure on the body's meridians (Ku-nye) increases the overall energy level of the body.
Phytotherapy.
For arthrosis, various herbal remedies are prescribed that speed up metabolism, increase the level of body heat, accelerate recovery processes in the body, have an anti-inflammatory effect and improve the functioning of the liver and kidneys.
Auxiliary means.
As auxiliary means, hirudotherapy, stone therapy, manual therapy and shock wave therapy are used.
Hirudotherapy has an anti-inflammatory effect and improves blood circulation.
Hot stone therapy increases body heat levels.
Shock wave therapy (SWT) improves local blood circulation, accelerates healing and restoration of the joint.
With the help of manual therapy, the doctor relieves the aching joint, increases the range of motion and mobility.
Diet for osteoarthritis
For arthrosis, heating and hot meals are indicated.
It is recommended to reheat foods such as fish, lamb, poultry, seafood, pumpkin, liver, nuts, as well as garlic, onions, ghee and sesame oil.
To increase the energy value of food, you should definitely consume spices (ginger, cinnamon, cardamom, cloves, pepper, turmeric, coriander, asafoetida, etc. ).
Hot dishes containing a lot of animal connective tissue, such as broths rich in bones and meat, are useful.
You should exclude cold foods, cool drinks, reduce the consumption of refreshing foods such as sugar, butter, milk and dairy products, sweets, citrus fruits, raw vegetables and leafy salads, semolina and legumes.
Prevention of osteoarthritis
To prevent arthrosis, you should avoid the factors that cause an imbalance underlying Bad Kan: refreshing diet, sedentary lifestyle (physical inactivity), exposure to cold, humidity.
Warming nutrition, physical activity, especially walking, outdoor games and physiotherapy exercises are useful.
Frequently asked questions about osteoarthritis
Are vitamin complexes useful for osteoarthritis?
Vitamin complexes influence metabolic processes in general. But they have no specific, preventive or therapeutic effect for joint diseases. To maintain general health and balance of the body, vitamins contained in foods are sufficient, provided that proper nutrition is provided.
Is there always inflammation with osteoarthritis?
No, not always. Osteoarthritis may be accompanied by arthritis, but the inflammation is secondary. Therefore, the use of NSAIDs (nonsteroidal anti-inflammatory drugs) for arthrosis does not always help and is often useless.
Is heat good for your joints?
Warming up for osteoarthritis helps improve blood circulation and is generally beneficial. But only in the absence of an acute inflammatory process. For arthritis, thermal procedures and warming are contraindicated.
How long does treatment for osteoarthritis last?
Usually, a course of treatment in a rehabilitation clinic consists of 10-15 complex sessions, which are carried out every other day and last 21-30 days. Afterwards there is a 6 month break. Six months later, an examination is carried out, on the basis of which it is decided to conduct a second course of treatment to improve and consolidate the results.




























































































